Diabetes affects about a third of all hospitalized patients and up to 50% of inpatients go on to experience hyperglycemia. Determining the optimal insulin dosage for patients, especially in the hospital environment, can be difficult due to the complex nature of their conditions and the fluctuating nature of their insulin requirements.
Despite strong evidence supporting the importance of adequate glycemic control, as well as detailed guidelines from major national organizations, many patients continue to have hypo- and hyperglycemia during their hospital stay. While this may be partially related to provider and patient-specific factors, system-based barriers continue to pose a major obstacle. Therefore, there's a need to go beyond merely discussing specific insulin protocols, or paper protocols which are still a norm, and provide guidance for effective models of care in the acute glycemic management of hospitalized patients.
What is a Glycemic Management Platform?
A glycemic management platform is a software-based system designed to assist healthcare providers in monitoring, managing, and optimizing the blood glucose levels of patients, particularly in clinical settings such as hospitals or other inpatient settings. The platform incorporates various tools, features, and functionalities to support the implementation of standardized protocols, facilitate data integration and analysis, provide decision support, and enhance communication and coordination among healthcare providers involved in glycemic management.
Why Replace Paper Protocols?
Traditional paper-based, linear insulin protocols have presented numerous challenges, including:
- Poor compliance
- High rates of hyperglycemia and hypoglycemia
- Prolonged time to achieve target glucose levels, and ultimately
- increased length of hospital stays
However, advanced inpatient glycemic management platforms are transforming the way healthcare professionals approach insulin dosing, offering a more efficient and effective solution to improve patient outcomes.
The key components and features of a glycemic management platform may include:
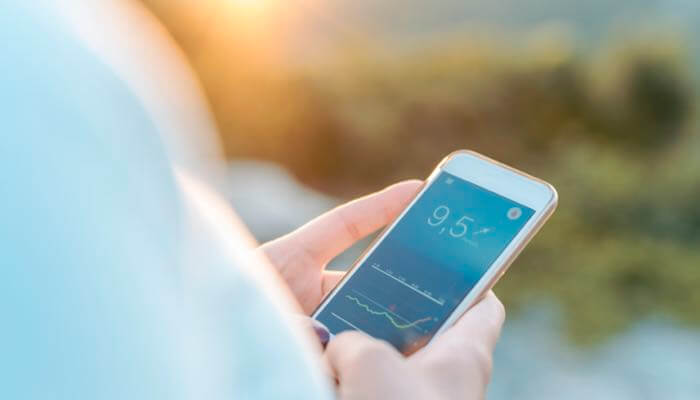
Glucose Monitoring: The platform integrates with bedside glucometers or other glucose monitoring devices to capture real-time blood glucose measurements. It allows for a seamless transfer of glucose data from these devices to the software system.
Data Integration: The platform may integrate with electronic health records (EHRs) and other data sources to aggregate and consolidate patient information, including glucose measurements, medication records, comorbidities, and other relevant data points.
Decision Support Tools: Glycemic management platforms often provide decision support tools that analyze patient-specific data and provide real-time recommendations and alerts to healthcare providers. These tools may assist in medication dosing, insulin administration, or other interventions based on established protocols and guidelines.
Standardized Protocols: The platform supports the implementation of standardized glycemic management protocols and guidelines across the clinical setting. It ensures consistent practices and adherence to evidence-based approaches for glycemic control.
Communication and Coordination: Glycemic management platforms facilitate communication and coordination among healthcare providers involved in a patient's care. They enable secure sharing of glucose data, treatment plans, and alerts, ensuring that all relevant team members have access to up-to-date information and can collaborate effectively.
Data Analysis and Reporting: The platform offers data analysis and reporting capabilities, allowing healthcare providers to examine glucose trends, outcomes, and performance metrics. It generates reports and provides analytics to support quality monitoring, research, and continuous improvement efforts.
Documentation and Documentation Integration: Glycemic management platforms streamline documentation processes by providing electronic forms or templates for recording glucose measurements, interventions, and outcomes. They may integrate with EHRs or other documentation systems to ensure accurate, timely, and efficient recording of glycemic management data.
Key Benefits of Glycemic Management Platforms
The benefits are numerous with new features and functionality being added. At a high level, key benefits reported by users include:
- Enhanced Patient Safety: An inpatient glycemic management platform provides real-time monitoring and analysis of patients' blood glucose levels, allowing for early detection and prevention of hypoglycemic or hyperglycemic episodes. This improves patient safety by reducing the risk of adverse events associated with poorly managed blood sugar levels.
- Improved Glycemic Control: The platform offers healthcare professionals access to comprehensive patient data, including historical blood glucose readings, insulin dosages, and meal information. With this information, clinicians can develop personalized treatment plans and make informed adjustments to insulin therapy, resulting in better glycemic control for patients.
- Time Efficiency: An inpatient glycemic management platform automates various aspects of glucose monitoring and data collection, streamlining the workflow for healthcare providers. It reduces manual documentation tasks and offers real-time alerts and notifications, enabling clinicians to prioritize and respond promptly to critical glucose-related events.
- Greater Consistency: The platform often includes decision support tools such as clinical guidelines and protocols for glycemic management. These tools assist healthcare professionals in making evidence-based decisions, reducing variations in care, and ensuring consistency in treatment approaches.
- Better Reporting: An inpatient glycemic management platform collects and analyzes data from multiple patients, providing valuable insights into glycemic patterns, trends, and outcomes. These analytics help identify areas for improvement, assess the effectiveness of interventions, and support quality improvement initiatives. Moreover, the platform generates comprehensive reports for auditing, research, and regulatory compliance purposes.
Potential Challenges
Establishing an inpatient glycemic management platform can be complex given various challenges associated with implementing new protocols, technologies, and practices in a hospital setting. Some of the primary challenges include:
Interdisciplinary Coordination: Inpatient glycemic management involves collaboration among multiple healthcare disciplines, including physicians, nurses, dietitians, pharmacists, and administrative staff. Coordinating efforts and ensuring consistent communication across these disciplines can be challenging, as each group might have different perspectives and priorities.
Change Management: Implementing new glycemic management protocols often requires a significant shift in clinical practices and workflows. Resistance to change from healthcare providers, staff, and even patients can hinder the successful adoption of the new platform.
Clinical Variation: Healthcare providers might have different approaches to glycemic management, leading to clinical variation in insulin dosing and monitoring practices. Establishing standardized protocols and ensuring adherence can be difficult, as some providers may be reluctant to relinquish their established practices.
Education and Training: Proper training and education are essential for all healthcare staff involved in the glycemic management process. Ensuring that nurses, physicians, and other staff members understand the new protocols, technologies, and best practices can be time-consuming and resource-intensive.
Data Integration: Many modern glycemic management platforms rely on electronic health records (EHR) and data integration to make informed decisions. Ensuring seamless integration between the platform and the hospital's existing EHR system can be technically complex and may require IT resources.
Technical Challenges: Implementing and maintaining a glycemic management platform may involve deploying new technologies, such as glucose monitoring systems, insulin pumps, and decision support algorithms. These technologies require proper setup, calibration, and ongoing maintenance, which can be technically challenging.
Patient Variability: Patients' responses to insulin and glycemic management can vary widely based on factors such as age, comorbidities, medication regimens, and dietary habits. Tailoring insulin dosing and management strategies to individual patient needs can be intricate and require constant adjustment.
Resource Allocation: Implementing a new glycemic management platform might necessitate additional resources, such as staff training, equipment, and personnel dedicated to overseeing the program. Hospital administrators need to allocate resources effectively to support the program's success.
Data Security and Privacy: Glycemic management platforms involve the collection and sharing of patient health data, which raises concerns about data security and patient privacy. Ensuring compliance with relevant data protection regulations is crucial.
Sustainability: After the initial implementation, sustaining the program's success over time can be challenging. Ensuring ongoing staff engagement, monitoring performance metrics, and making necessary adjustments to protocols and practices are essential for the long-term effectiveness of the platform.
Addressing these challenges requires a combination of effective leadership, clear communication, robust training programs, collaboration among different healthcare teams, and ongoing evaluation and improvement of the glycemic management platform.
Inpatient Glycemic Management Platform Options
There are a number of platforms for consideration including:
Glucommander from Glytec: Glucommander is an FDA-cleared insulin management software that provides personalized insulin dosing recommendations and maximizing workflow efficiency for doctors and nurses. Glucommander helps providers manage patients across the continuum of care with support for intravenous, subcutaneous, and outpatient insulin management as well as the transitions between these stages.
GlycoStabilizer: The GlucoStabilizer FDA- cleared system enables providers to reduce the frequency, risk, and cost of hyperglycemia, hypoglycemia, and glycemic variability for hospitalized patients.
EndoTool from Monarch: An FDA-cleared clinical decision support platform, the EndoTool Glucose Management System is suited to all hospital units -- critical care, non-critical care and observation alike -- as well as emergency departments, and has multiple dosing modes to support both intravenous and subcutaneous insulin.
All offer varying features and each should be evaluated to determine the one that's best for your inpatient facility and needs.
Practice Pearls from Shana Nicholson RN, CDCES, MLDE, PCCN
Shana recently played a pivotal role in the Glucommander roll-out team for her inpatient facility. Here are her key insights and recommendations for other healthcare providers looking to implement a system.
For Providers:
- Identification of Provider Champions is crucial to promote Glucommander and educate about the importance of the practice change.
- Provider education, including in-person and virtual demonstrations, needs to encompass the "WHY" of implementing Glucommander to reduce hypoglycemia rates and standardize protocols in alignment with best practices as defined by the ADA, among other factors.
- Utilization of the Glytec Inpatient Insulin Dose Calculator, which should be embedded in the order sets, is paramount. The Dose Calculator considers the patient's weight, home regimen (TDD), if applicable, and calculates a percentage reduction. This assists providers in informed decision-making regarding initial orders and starting doses.
- Glucommander titrates insulin doses up or down based on previous fasting or premeal blood glucose values to cater to the patient's specific needs. Insulin titration has a maximum of 30%, so initiating insulin at excessively high or low doses can cause delays in reaching the target blood glucose. (The importance of starting with an informed dose cannot be stressed enough for the algorithm's efficient functioning.) Providers have the ability to customize and edit insulin orders as needed. They should also review daily trends to make informed decisions.
For Nurses
- Identifying Nurse Champions to assist frontline staff in adapting to the new process/workflow is crucial.
- Providing in-person and virtual education/demonstrations to reinforce learning and the end-to-end workflow is imperative. This education should also explain the rationale behind the new approach.
- Ensuring that nurses have a solid foundation in the appropriate treatment of inpatient diabetes best practices is essential.
- Understanding the best practice when concerned about an insulin dose is crucial. Rather than merely withholding the dose, nurses should call the provider, provide background information, share previous doses and the patient's response, and request dose adjustments as necessary.
For All
- Education on the importance of the meal triad involving POC blood glucose testing, meal tray delivery, and insulin administration must be a coordinated and timely effort for optimization. This collaboration involves nursing, assistants, and food service.
- As mealtime insulin is determined by CHO intake, resources should be available to assist staff in calculating CHO counts.
- Utilizing a command center with around-the-clock coverage to assist staff during the implementation phase contributes to success.
Overall, this program is excellent for managing inpatient blood glucose for appropriate patients in the hospital. With proper ordering, achieving blood glucose within the target range becomes quicker and safer, with fewer deviations. Unfortunately, if patients are started with excessively high or low initial insulin doses, reaching the target blood glucose is more challenging.
Final Thoughts
Implementing a glycemic management platform in an inpatient setting can significantly enhance patient care, improve safety, optimize glycemic control, and facilitate data-driven decision-making. It promotes standardization, coordination, and communication among healthcare providers, ultimately leading to better patient outcomes and improved overall care quality.
But keep in mind, like most platforms, a strong team and full organizational support are required to implement, rollout and maintain these systems. Your organization will get out of it what it puts into it.


 Guidance on clinical assessment, adjustments, report interpretation and key education. Designed to be used during clinic visits.
Guidance on clinical assessment, adjustments, report interpretation and key education. Designed to be used during clinic visits.-(3).jpg?sfvrsn=16486d59_5)
 Proper basal insulin initiation and titration can help reduce therapeutic inertia and engage patients in their diabetes management. Find videos, podcasts and other resources to fine tune your knowledge.
Proper basal insulin initiation and titration can help reduce therapeutic inertia and engage patients in their diabetes management. Find videos, podcasts and other resources to fine tune your knowledge.
 An overview of Glycemic Management Platforms that answers key questions including: What are they? What to consider? How can my inpatient facility benefit and more.
An overview of Glycemic Management Platforms that answers key questions including: What are they? What to consider? How can my inpatient facility benefit and more.


 Certificate programs, webinars and courses related to cardiometabolic health and diabetes. Topics include weight loss, treatments, lifestyle enhancements, the latest technological advancements and more.
Certificate programs, webinars and courses related to cardiometabolic health and diabetes. Topics include weight loss, treatments, lifestyle enhancements, the latest technological advancements and more. Find danatech's interactive diabetes technology tools for point-of-care, insurance coverage and more.
Find danatech's interactive diabetes technology tools for point-of-care, insurance coverage and more.