Basal Insulin as a Tool for Empowerment
People with diabetes who are more engaged in their self-management are more likely to make progress toward meeting their goals.
It can be frustrating not being able to reduce glucose despite robust efforts made to improve activity levels and eating patterns.
Feelings of disappointment can lead people to disengage with their diabetes management.
Basal insulin is a treatment that can be safely self-titrated with initial training and increased or decreased in small increments to achieve fasting glucose targets.
Including basal insulin in the treatment plan in this way can increase engagement and confidence for the person with diabetes who needs to add insulin.
Self-titration as Part of the Treatment Plan
When fasting glucose is higher than the target goal (>130mg/dl), basal insulin is a valuable tool for lowering morning glucose. Typically, the main goal of using basal insulin is to bring fasting glucose down slowly and safely to reduce the chances of hypoglycemia. Empowering the person to reduce the dose when they notice a pattern of low glucose supports their autonomy and may achieve a safe level more quickly. Increased participation in sports, walking and other outdoor activities as well as weight loss, lower carbohydrate intake or periods of fasting all necessitate a decrease in insulin dose. Scheduling a spontaneous provider visit just to lower the basal insulin dose can be inconvenient when it may be incorporated safely by the patient with a self-titration plan.
Basal Insulin as a Tool to Lower A1C
Since Type 2 diabetes is progressive, we know that glucose will increase over time (sometimes more abruptly) and often remains high until a scheduled medical appointment. Basal insulin can change this trajectory and mitigate elevations between appointment times, especially with safe self-titration. Achieving fasting glucose targets with basal insulin can lead to a 1-4% or higher reduction in A1C and a reduced risk of diabetes-related complications (Lovre & Fonseca, 2015).
Basal Insulin Types
There are several types of basal insulin and although they are all considered long-acting insulins, they may have different durations of action or concentration as seen below in this chart:
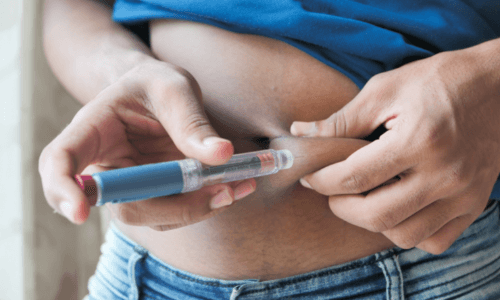
Basal insulin can be delivered subcutaneously via pen or a vial and syringe. Using a vial and syringe may be more difficult for people with poor vision or dexterity. Insulin pens make selecting and administering the right dose easier by allowing the user to dial up the dose, providing audible clicks for each unit or two (depending on the pen), and having visual confirmation of delivery of the dose via a dosing window. Insulin pens come in both disposable and reusable forms as well as connected insulin pens, which connect to data platforms and apps and have memory capabilities and reminder alerts for the user.
According to ADA guidelines, a starting dose of 0.1-0.2 units per kilogram of body weight is recommended (ElSayed et. al., 2023). Assessing fasting glucose values is a way to determine which starting dose is needed. Basal insulin is indicated when fasting glucose is consistently above 130 (except for patients with gestational diabetes). If fasting glucose is closer to target range, you may start with 0.1 units/kg. Whereas if fasting glucose is much further from target range, starting with 0.2 units/kg as an initial dose is reasonable.
Since basal insulin such as glargine typically lasts for 24 hours, timing does not need to be limited to the evening or the morning; it can be taken at whatever time is most convenient for the patient’s schedule.
Some people may have more chaotic mornings or evenings that make it difficult to take the insulin consistently, so it’s important to ask their preference. Using ultra-long-acting basal insulin such as Tresiba or Toujeo offers the option of once-daily flexible dosing, allowing for a longer window (3-8 hours from a missed dose) to take their dose without losing background insulin coverage or stacking insulin with their next dose (Riddle et. al., 2016).
Basal Insulin Titration Steps
First, ensure the person is monitoring their fasting glucose. They will need this information to titrate their basal insulin dose safely and effectively.
Next, select a fasting glucose target range such as ADA’s glycemic recommendation of 80-130 mg/dl. This target can be personalized for safety and to better match the person’s goals. A higher target range such as 100-140mg/dl may be used to further reduce the risk for hypoglycemia for patients with hypoglycemia unawareness or the elderly population (ElSayed et. al., 2023).
Next, titrate based on fasting glucose readings. If fasting glucose remains higher than the target range after the starting dose of basal insulin, the dose should be increased by 2 units every 2-4 days if the result is higher than the goal. If the fasting glucose is less than the target range, the dose should be reduced by 2 units every 2 days to prevent hypoglycemia.
An EMR smart phrase that can be personalized based on a patient’s goal may look like this:
Start ___ (20) units of basal insulin every (morning/evening). Aim for morning blood sugars from ___-___ (90-130) on average. Every __ (3) days you are higher than __ (130), increase the dose by 2 units. Every __ (2) days you are less than 100 in the morning, decrease the dose by 2 units.
Other titration tips
For patients more sensitive or less sensitive to insulin, the insulin titration unit amount can be changed, such as in 1-unit or 4-unit increments instead of 2 units.
When changing from glargine to detemir or from ultra-long-acting insulin to glargine, or vice versa, the dose conversion remains one-to-one.
If a patient is giving twice daily injections of basal insulin, typically the doses can be added together to take once daily by switching to ultra-long-acting basal insulin.
If a patient is not reaching target fasting glucose levels despite the recommendations above, check their injection technique and injection site to ensure proper absorption.
If A1C remains above goal and fasting glucose is within the desired range, a medication that targets postprandial glucose may be needed to reduce A1C further. As a general rule, this should be considered when the total basal dose reaches approximately 0.5u/kg (Reid et. al., 2016).
For patients with greater concern for hypoglycemia, those using glargine and detemir had lower occurrences of hypoglycemia than patients using NPH insulin. Likewise, patients using Toujeo or Tresiba insulins had lower occurrences of hypoglycemia than patients using glargine U-100 or detemir (ElSayed et. al., 2023).
Summary
Basal insulin is very effective in reducing fasting glucose and can be more effective on a consistent basis and in between medical visits when patients are given a titration plan.
Educating patients to change their dose to improve their fasting glucose may increase their engagement and confidence in managing diabetes, as well as improve their long-term glycemic management.
Start with an individualized fasting glucose target range and titrate the dose every 2-4 days if outside of the target range.
Check injection technique or injection site for scar tissue or lipohypertrophy if fasting glucose is not in target.
When switching to a different basal insulin, there is a 1:1 conversion rate regardless of using a U-100, U-200, or U-300 basal insulin.
Ultra-long-acting basal insulins can help reduce the number of injections, offer patients flexibility in their dose timing, and reduce the chance of hypoglycemia. There is no significant risk of stacking insulin with ultra-long-acting basal insulins when given every 24 hours (Davis et. al., 2018).
Do not increase basal insulin further if fasting glucose is in the goal range yet A1C remains high. A medication that targets postprandial glucose is needed instead.
References
Davis, C. S., Fleming, J. W., Malinowski, S. S., Brown, M. A., & Fleming, L. W. (2018). Ultra-long-acting insulins: A review of efficacy, safety, and implications for practice. Journal of the American Association of Nurse Practitioners, 30(7), 373-380.
ElSayed, N. A., Aleppo, G., Aroda, V. R., Bannuru, R. R., Brown, F. M., Bruemmer, D., ... & Gabbay, R. A. (2023). 6. Glycemic targets: standards of care in diabetes—2023. Diabetes Care, 46(Supplement_1), S97-S157.
Lovre, D., & Fonseca, V. (2015). Benefits of timely basal insulin control in patients with Type 2 diabetes. Journal of Diabetes and its Complications, 29(2), 295-301.
Reid, T., Gao, L., Gill, J., Stuhr, A., Traylor, L., Vlajnic, A., & Rhinehart, A. (2016). How much is too much? Outcomes in patients using high-dose insulin glargine. International journal of clinical practice, 70(1), 56–65. https://doi.org/10.1111/ijcp.12747
Riddle, M. C., Bolli, G. B., Home, P. D., Bergenstal, R. M., Ziemen, M., Muehlen-Bartmer, I., ... & Yki-Järvinen, H. (2016). Efficacy and safety of flexible versus fixed dosing intervals of insulin glargine 300 U/mL in people with Type 2 diabetes. Diabetes Technology & Therapeutics, 18(4), 252-257.


 Guidance on clinical assessment, adjustments, report interpretation and key education. Designed to be used during clinic visits.
Guidance on clinical assessment, adjustments, report interpretation and key education. Designed to be used during clinic visits.-(3).jpg?sfvrsn=16486d59_5)
 Proper basal insulin initiation and titration can help reduce therapeutic inertia and engage patients in their diabetes management. Find videos, podcasts and other resources to fine tune your knowledge.
Proper basal insulin initiation and titration can help reduce therapeutic inertia and engage patients in their diabetes management. Find videos, podcasts and other resources to fine tune your knowledge.
 An overview of Glycemic Management Platforms that answers key questions including: What are they? What to consider? How can my inpatient facility benefit and more.
An overview of Glycemic Management Platforms that answers key questions including: What are they? What to consider? How can my inpatient facility benefit and more.


 Certificate programs, webinars and courses related to cardiometabolic health and diabetes. Topics include weight loss, treatments, lifestyle enhancements, the latest technological advancements and more.
Certificate programs, webinars and courses related to cardiometabolic health and diabetes. Topics include weight loss, treatments, lifestyle enhancements, the latest technological advancements and more. Find danatech's interactive diabetes technology tools for point-of-care, insurance coverage and more.
Find danatech's interactive diabetes technology tools for point-of-care, insurance coverage and more.